by Andrea Kelly D.C Chiropractor

What is Osteoporosis?
Osteoporosis (literally translated as ‘porous bones’) is described by the World Health Organisation (WHO) as a progressive systemic skeletal disease characterised by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture.
Every year in the UK more than 500,000 broken bones are caused by osteoporosis and the most common locations of these fractures are the spine, hip and wrist. More than 1 in 3 women, and 1 in 5 men, will sustain one or more osteoporotic-related fractures in their lifetime.
Fractures can cause substantial pain and severe disability, often leading to a reduced quality of life, and hip and vertebral fractures are associated with decreased life expectancy.
Here at North Down Chiro&Physio, patients present to us with a large variety of complaints, and our therapists will always consider the presence of osteoporosis, an osteoporotic fracture or major risk factors of osteoporosis (whether or not it is related to the presenting condition).
We aim to identify patients with significant risk factors prior to loss of bone density and to provide early preventative support and advice. We also strive to identify those at risk of osteoporotic fractures and support them to make the necessary lifestyle and practical changes to help limit this risk, as well as making appropriate referrals for further investigations and management.
Given that chiropractic involves hands-on treatment, understanding a patient’s bone health is of particular importance to us. Many of our patients have osteopenia and osteoporosis and we use modified techniques to treat these patients safely and effectively, based on each individual patient’s initial assessment.

The modifiable risk factors of osteoporosis include exercise, weight (BMI), smoking, alcohol intake, diet and supplements. Guidance to maintain good bone health is as follows:
Aim to do weight bearing exercise such as: walking; jogging; weight training; climbing stairs; tennis, trampolining and dancing. These are useful as they help to stimulate bone formation. Swimming and cycling are less useful as they are non-weight bearing.
Tai Chi and yoga are helpful for improving balance, co-ordination and posture, as are fall prevention classes which you can be referred to.
Under 65 year olds should aim to do 30 minutes of moderate intensity exercise 5 days per week (including muscle building exercises 2 days per week). Low force dynamic weight bearing exercise such as Tai Chi is associated with reduced decline in bone mineral density in over 65 year olds.
Try to maintain a healthy body mass index (BMI) of over 20 kg/m2, as low BMI is associated with an increased risk of osteoporosis.
Do not smoke and limit alcohol intake to less than 2 units a day.
Try to consume a healthy balanced diet which contains adequate intake of dietary calcium and vitamin D. Daily calcium intake should be between 700mg and 1200mg, preferably from the diet, but supplemented if necessary. The Royal Osteoporosis Society offer a ‘Calcium Calculator’ and food chooser, which can be helpful in maximising dietary calcium.
Consider Vitamin D supplementation (whole population), at least during the winter months. For postmenopausal women and men over 50 who are at risk of osteoporotic fracture, a daily vitamin D supplement of 20µg (800 IU) is advised since it aids calcium absorption.
Limit coffee intake to 4 cups per day, as observational studies have shown an increased fracture risk with high intakes of coffee.
Vitamin A may have a negative effect on bone density, therefore avoid Vitamin A supplements and limit liver intake (once per week max).
References:
Diagnosis and management of osteoporosis. Dr Barbara Noble
Royal College of Chiropractors. Chiropractic Quality Standard: Osteoporosis

More Posts
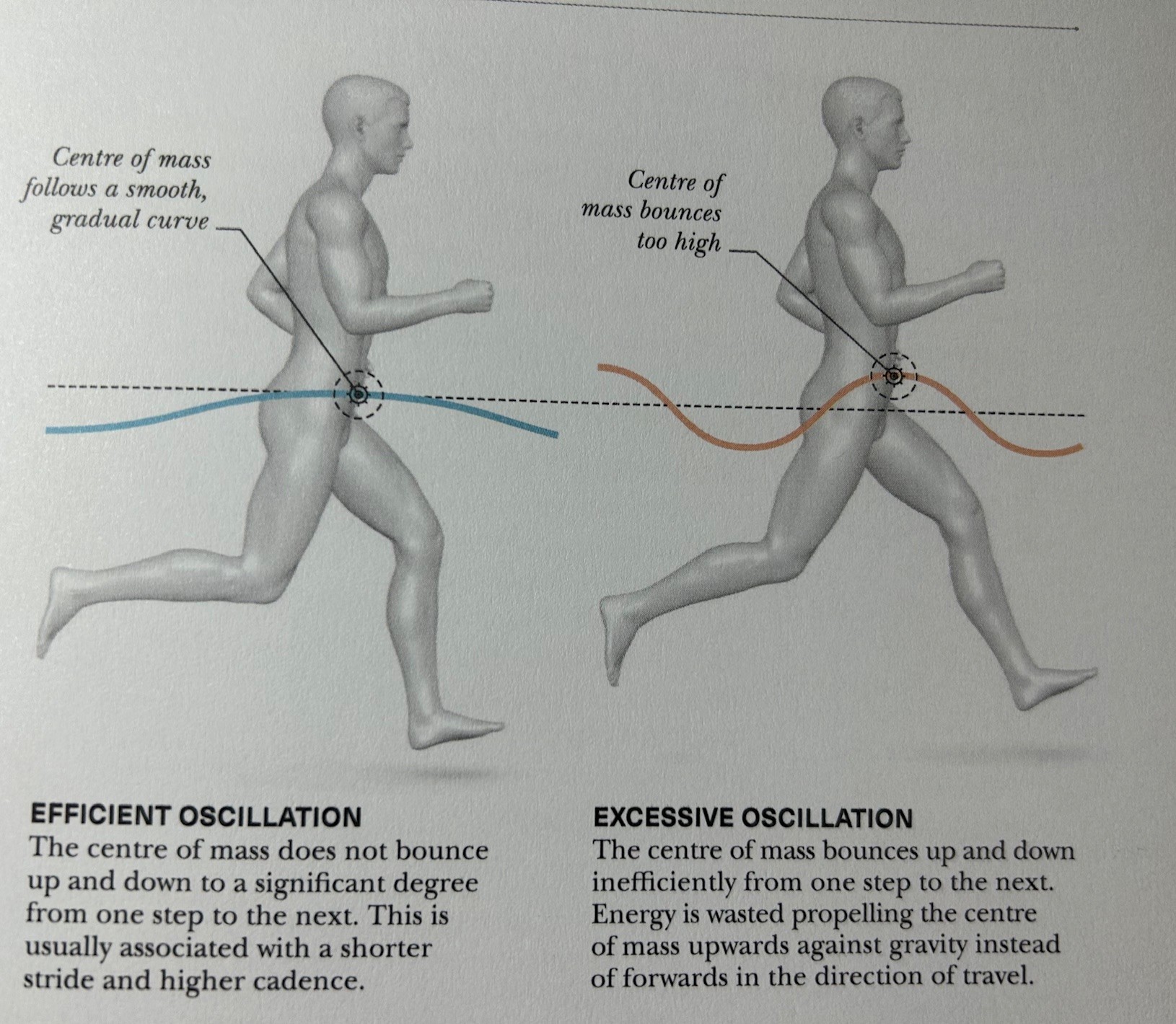
Running blog: Part two

Running and Injury mechanics

Physiotherapy for Runners with Hip Pain: How to Get Back on Track

Parenting ‘Perils’
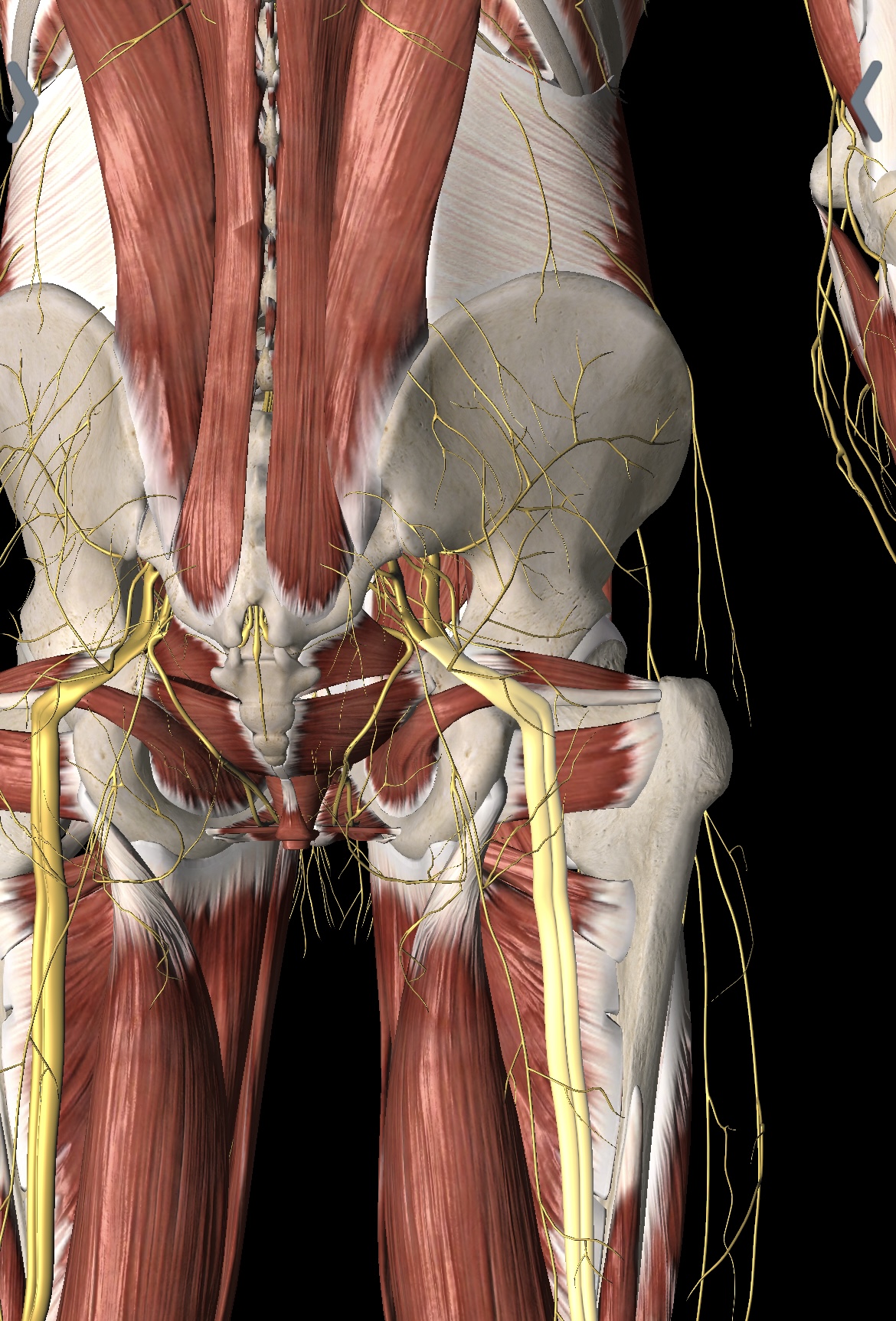
Sciatica explained

Physiotherapy for Jaw pain/TMJ

Pilates now available

Physiotherapy, Pain and hairdressing



